June 20, 2019 weblog
Imaging results, health data combine in AI model to predict breast cancer
Women know the drill: Breast cancer is too commonly a cancer diagnosis to be ignored, as early detection could make a difference. While false positives may cause an enormous amount of undue stress, false negatives have an impact on how early a cancer is detected and subsequently treated.
Earlier detection might give the person more options for successful intervention and therapies with her condition still at its early stage.
A team at IBM Research have turned to artificial intelligence to see if they could come up with a solution that achieves an impressive level of accurate detection of breast cancer, and their results are encouraging.
In an IBM Research Blog post, IBM Research's Michal Chorev described the team's goals, efforts and outcomes.
He said that "as the first algorithm of its kind to learn and make decisions from both imaging data and a comprehensive patient's health history, our model was able to correctly predict the development of breast cancer in 87 percent of the cases it analyzed, and was also able to correctly interpret 77 percent of non-cancerous cases."
The addition of clinical data to the mammograms significantly increased the model's AUROC and sensitivity.
"When based on clinical data alone, our model obtained an AUROC of 0.78, improving breast cancer risk prediction in comparison to common risk models like Gail model. Moreover, we were able to identify clinical factors that may possibly contribute to elevated risk and which were not previously used by other models, such as white blood cell profiles and thyroid function tests."
First off, the team at IBM Research–Haifa hypothesized that a model combining machine learning and deep learning could be applied to assess breast cancer at a level both comparable to radiologists and with the capabilities to be accepted into clinical practice as a second reader.
As it turned out, it seems as if predicting breast cancer with AI with something close to radiologist-level accuracy was not a mere flight of the imagination.
The work of these IBM researchers appears in Radiology and it discusses the AI model that can predict the development of malignant breast cancer in patients within the year with favorable accuracy rates. "More accurate prediction could hold the potential to reduce the number of women being sent for unnecessary tests—or experiencing the trauma of being needlessly assigned as high risk—by traditional models."
This would not be the first time research turned to AI for such purposes. Researchers had already been building prediction models based on artificial intelligence, said Adnan Farooqui in Ubergizmo.
Fingas made the distinction as to what is novel about this work. While there were are already AI prediction methods, either they relied on mammogram images or they focused on medical records. "IBM's stands out by using both."
Chorev blogged that this was "the first algorithm of its kind to learn and make decisions from both imaging data and a comprehensive patient's health history."
How comprehensive? The answer lies in how IBM trained its AI, with anonymized mammography images linked to biomarkers (such as reproductive history) and clinical data, said Fingas. According to the IBM Research blog, they trained the algorithm on 9,611 mammograms and health records of women, with two objectives: (1) to predict biopsy malignancy and (2) differentiate normal from abnormal screening examinations.
"Through IBM research partners Maccabi Health Services and Assuta Medical Center, two large health providers in Israel, our team was able to obtain a large set of de-identified, voluntarily collected mammography images that were also linked to rich and detailed record of the corresponding individual's clinical data—such as a history of any cancer diagnoses, pregnancy history and status of menopause."
What's more, there were traits that one would not discover in imagery alone, e.g., iron deficiencies and thyroid function. Overall, wrote Chorev, this is all about an "astonishing amount of data" providing "a deep pool of information from which our machine learning models could learn."
The amount of data allowed the algorithms "to connect patterns and trends that may not have been possible otherwise." Data involved biopsies, lab tests, cancer registries and codes from other diagnoses and procedures.
The team sees this AI model not as a replacement for radiologists but as a second set of eyes. In addition to human assessments, "the accuracy is good enough that it could serve as a 'second set of eyes,' according to IBM."
It could verify a radiologist's prognosis and reduce the chances of patients being sent in for unnecessary follow-up tests.
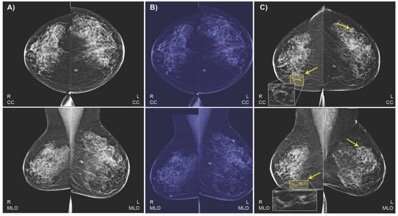
Analyzing mammograms is a challenging task. The differences between lesions and background could be subtle: there are multiple types of possible findings in shape, size, color, texture and other factors.
Radiology Business: Though the team's model did not necessarily outperform radiologists, its performance did fall in "the acceptable range of radiologists for breast cancer screening."
For further reading, their paper "Predicting Breast Cancer by Applying Deep Learning to Linked Health Records and Mammograms" appears in Radiology.
More information: www.ibm.com/blogs/research/201 … gist-level-accuracy/
Ayelet Akselrod-Ballin et al. Predicting Breast Cancer by Applying Deep Learning to Linked Health Records and Mammograms, Radiology (2019). DOI: 10.1148/radiol.2019182622
© 2019 Science X Network
















